Blood cells are made a little differently than you might think. This could have implications for the fight against cancer
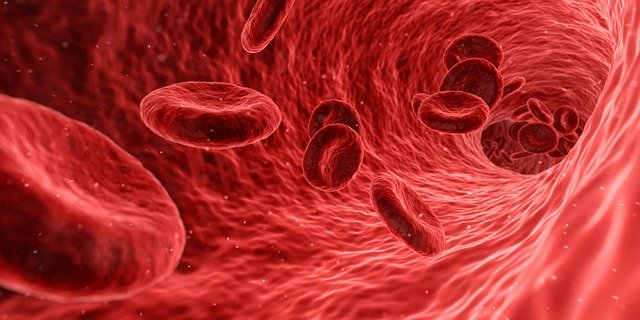 blood cells form differently than previously thought, researchers at Boston Children's Hospital report in Nature. In studies on mice, they have shown that such cells are not made of one, but of two kinds of progenitor cells are formed. This in turn can be of enormous importance for the treatment of Blood cancer, for bone marrow transplants and for the development of immunology.
blood cells form differently than previously thought, researchers at Boston Children's Hospital report in Nature. In studies on mice, they have shown that such cells are not made of one, but of two kinds of progenitor cells are formed. This in turn can be of enormous importance for the treatment of Blood cancer, for bone marrow transplants and for the development of immunology.
So far it has been assumed that most of our blood originates from a small number of cells that become blood stem cells, also known as hematopoietic stem cells. To our astonishment, we discovered that there is a second group of progenitor cells that are not derived from stem cells. It is they who make up most of the blood in our body from fetus to early adulthood, after which their contribution to blood formation decreases," says senior physician Fernando Camargo.
The newly discovered cells are embryonic multipotent progenitor cells. The researchers are now examining whether their discovery, which they made in mice, can also be applied to humans. If this is the case, it could help develop methods of boosting the immune system in older people, new insights into blood cancers, especially in children, gain or improved methods for bone marrow transplant to allow.
Image source: Pixabay; Which
We're also trying to understand why these cells disappear in middle age. If we're successful, maybe we can manipulate them to rejuvenate the immune system, says Camargo. The scientist is also excited about the possibility of better treatment for blood cancer. He notes that many of these diseases are age specific. myeloid leukemias occur mainly in older people. Maybe, according to Camargo, they come from blood stem cells away. And lymphoid leukaemias, which primarily affect children, can arise from embryonic multipotent progenitor cells. We are attempting to understand the consequences of mutations leading to leukemia and their impact on stem cells and embryonic multipotent progenitor cells in mice. We want to see if these cancers occur in different cells, the scientist adds.
The discovery could also have implications for bone marrow transplants. When we transplanted bone marrow into mice, we found that the embryonic pluripotent cells did not implant well and survived only a few weeks. Meanwhile, if we could add a gene to these cells to prolong their survival, these cells could be a better cell source for transplantation. This is because they are more common than stem cells and mainly in young donors Lymphocytes produce, resulting in a better reconstitution of the Immune system and fewer post-transplant complications, Camargo explains.